Betabloqueantes
Revisado por la Dra. Rachel Hudson, MRCGPÚltima actualización por Dr Rosalyn Adleman, MRCGPÚltima actualización 23 mar 2023
Satisface las necesidades del paciente directrices editoriales
- DescargarDescargar
- Compartir
- Idioma
- Debate
Los betabloqueantes son medicamentos que se utilizan para tratar diversas afecciones. Su nombre completo correcto es bloqueantes beta-adrenoceptores (o bloqueantes beta-adrenérgicos), pero normalmente se denominan simplemente betabloqueantes.
En este artículo:
Seguir leyendo
¿Cómo actúan los betabloqueantes?
Los betabloqueantes actúan bloqueando la transmisión de determinados impulsos nerviosos. Los extremos de algunos nervios liberan una sustancia química (neurotransmisor) llamada noradrenalina cuando se estimula el nervio. Esta sustancia química estimula los receptores beta-adrenérgicos.
Estos receptores son estructuras diminutas que se encuentran en las células de diversas partes del cuerpo, como el corazón, el cerebro y los vasos sanguíneos. Cuando se estimulan estos receptores, provocan diversos efectos. Por ejemplo, los impulsos nerviosos que llegan al corazón pueden estimular los receptores beta-adrenérgicos de las células cardiacas. Esto provoca un aumento de la fuerza y la frecuencia de los latidos del corazón. Esto puede acelerar los latidos y elevar la tensión arterial.
Los receptores beta-adrenérgicos también son estimulados por la adrenalina (epinefrina), una hormona que circula por el torrente sanguíneo. La adrenalina se fabrica en la glándula suprarrenal. El nivel de adrenalina en sangre puede variar. Por ejemplo, puede liberar mucha adrenalina en el torrente sanguíneo cuando está asustado o ansioso, lo que puede provocar un aumento del ritmo cardíaco y otros efectos.
Los betabloqueantes "se asientan" sobre los receptores betaadrenérgicos e impiden (bloquean) que se estimulen. Así, por ejemplo, si se bloquean los receptores betaadrenérgicos del corazón, se reducen la fuerza y la frecuencia de los latidos.
Tipos de betabloqueantes
Existen varios tipos de betabloqueantes:
Cada tipo tiene una o varias marcas.
Seguir leyendo
¿Para qué se utilizan los betabloqueantes?
Afecciones cardiacas y vasculares
Debido a su efecto sobre las células del corazón, los betabloqueantes pueden utilizarse para:
Controlar ciertos ritmos cardíacos anormales (arritmias), en particular aquellos en los que el latido es demasiado rápido. Una arritmia frecuente es la fibrilación auricular. Los betabloqueantes suelen utilizarse para controlar la frecuencia cardíaca rápida en la fibrilación auricular. Los antagonistas del calcio son un medicamento alternativo que puede utilizarse para este problema.
Ayuda a tratar la insuficiencia cardíaca.
Otras condiciones
Dado que los receptores betaadrenérgicos se encuentran en otras partes del cuerpo, los betabloqueantes también se utilizan para otras afecciones. Entre ellas se incluyen:
Glaucoma. Los colirios betabloqueantes reducen el líquido que produce en la cámara anterior del ojo. Esto reduce la presión en el ojo.
La ansiedad. Los betabloqueantes no reducen la ansiedad en sí, pero pueden reducir algunos de sus síntomas. Por ejemplo, pueden reducir las sacudidas (temblores) y la frecuencia cardiaca acelerada.
Glándula tiroides hiperactiva. Los betabloqueantes pueden ayudar a reducir síntomas como el temblor y a disminuir la frecuencia cardiaca.
Migraña. Los betabloqueantes pueden reducir el número de crisis de migraña si éstas son frecuentes.
Temblores: los betabloqueantes pueden utilizarse en temblores benignos de la mano que no tengan otra causa subyacente y causen problemas importantes en las actividades cotidianas.
Efectos secundarios de los betabloqueantes
La mayoría de las personas que toman betabloqueantes no tienen efectos secundarios, o éstos son leves. Sin embargo, debido a su acción en diversas partes del cuerpo, algunas personas tienen efectos secundarios no deseados. Los efectos secundarios de los betabloqueantes son::
A veces, la frecuencia cardiaca puede ir demasiado lenta. Esto puede provocar mareos o sensación de desmayo.
Si padece diabetes, debe tener en cuenta que los betabloqueantes pueden atenuar las señales de alarma de una bajada de azúcar(hipoglucemia ). Por ejemplo, es posible que no tenga la sensación de latidos cardíacos rápidos, fuertes o irregulares (palpitaciones) o temblores, que suelen aparecer cuando el nivel de azúcar en sangre es demasiado bajo.
A algunas personas se les enfrían las manos y los pies cuando toman betabloqueantes. Esto se debe a que pueden estrechar (constreñir) los vasos sanguíneos pequeños y reducir la circulación a la piel de las manos y los pies.
En algunas personas se produce cansancio, depresión, incapacidad para lograr una erección adecuada (impotencia), sueños vívidos, pesadillas y otros problemas para dormir.
Existen indicios de que los betabloqueantes pueden provocar el desarrollo de diabetes de tipo 2 en algunas personas.
A algunas personas asmáticas se les recomienda no tomar betabloqueantes. Si padece asma o algo similar, coméntelo con su médico de cabecera.
Lo anterior no es una lista completa de los posibles efectos secundarios, pero menciona los principales que pueden producirse. Lea el prospecto de su marca para conocer la lista completa de posibles efectos secundarios y precauciones.
Seguir leyendo
¿Cuánto tiempo se pueden tomar los betabloqueantes?
La duración del tratamiento depende del motivo por el que se toma el betabloqueante. Algunas personas sólo necesitan tomar betabloqueantes durante unas semanas o meses, por ejemplo, si tiene una tiroides hiperactiva. Algunas personas necesitan tomar betabloqueantes durante el resto de su vida, por ejemplo, después de un ataque al corazón (infarto de miocardio).
¿Quién no puede tomar betabloqueantes?
No puede tomar un betabloqueante si padece ciertas afecciones, entre las que se incluyen:
Asma.
Insuficiencia cardíaca no controlada.
Frecuencia cardíaca muy lenta(bradicardia).
Presión arterial baja (hipotensión).
Ciertos problemas del ritmo cardíaco, como el síndrome del seno enfermo.
Patient picks for Heart and blood medicines

Tratamiento y medicación
Inhibidores de la ECA
ACE inhibitors are medicines that are used mainly in the treatment of high blood pressure (hypertension) and heart failure. They are also used in some people with diabetes, for some forms of kidney disease, and after a heart attack, to help protect the heart. They have a variety of effects on the body. Their ability to relax blood vessels is one of the most important. The side-effects most commonly associated with ACE inhibitors are usually minor. A common side-effect is a persistent dry cough.
por el Dr. Toni Hazell, MRCGP
Tratamiento y medicación
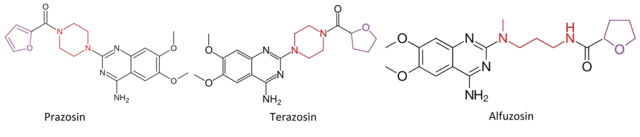
Alfabloqueantes
Alpha-blockers are medicines that are mainly used to treat high blood pressure (hypertension) and problems with passing urine in men who have enlargement of the prostate gland. Prostate gland enlargement is also called benign prostatic hyperplasia (BPH).
por el Dr. Doug McKechnie, MRCGP
Lecturas complementarias y referencias
- HipertensiónNICE Pathway, agosto de 2011
- Síndrome coronario agudo; Red escocesa de directrices intercolegiales - SIGN (2016)
- Fibrilación auricular: diagnóstico y tratamiento; directriz NICE (abril 2021 - última actualización junio 2021)
- 2021 Directrices de la ESC para el diagnóstico y tratamiento de la insuficiencia cardíaca aguda y crónicaDesarrollado por el Grupo de Trabajo para el diagnóstico y tratamiento de la insuficiencia cardíaca aguda y crónica de la Sociedad Europea de Cardiología (ESC) Con la contribución especial de la Asociación de Insuficiencia Cardíaca (HFA) de la ESC
- Migraña; NICE CKS, August 2025 (UK access only)
Seguir leyendo
Historia del artículo
La información de esta página ha sido redactada y revisada por médicos cualificados.
Próxima revisión prevista: 21 de marzo 2028
23 Mar 2023 | Última versión

Pregunte, comparta, conecte.
Explore debates, formule preguntas y comparta experiencias sobre cientos de temas de salud.

¿Se encuentra mal?
Evalúe sus síntomas en línea de forma gratuita
Suscríbase al boletín informativo para pacientes.
Tu dosis semanal de consejos de salud claros y fiables, redactados para ayudarte a sentirte informado, seguro y en control.
Al suscribirte, aceptas nuestra Política de privacidad. Puedes darte de baja en cualquier momento. Nunca vendemos tus datos.